5 Key Differences Between Fee-for-Service and Value-Based Care
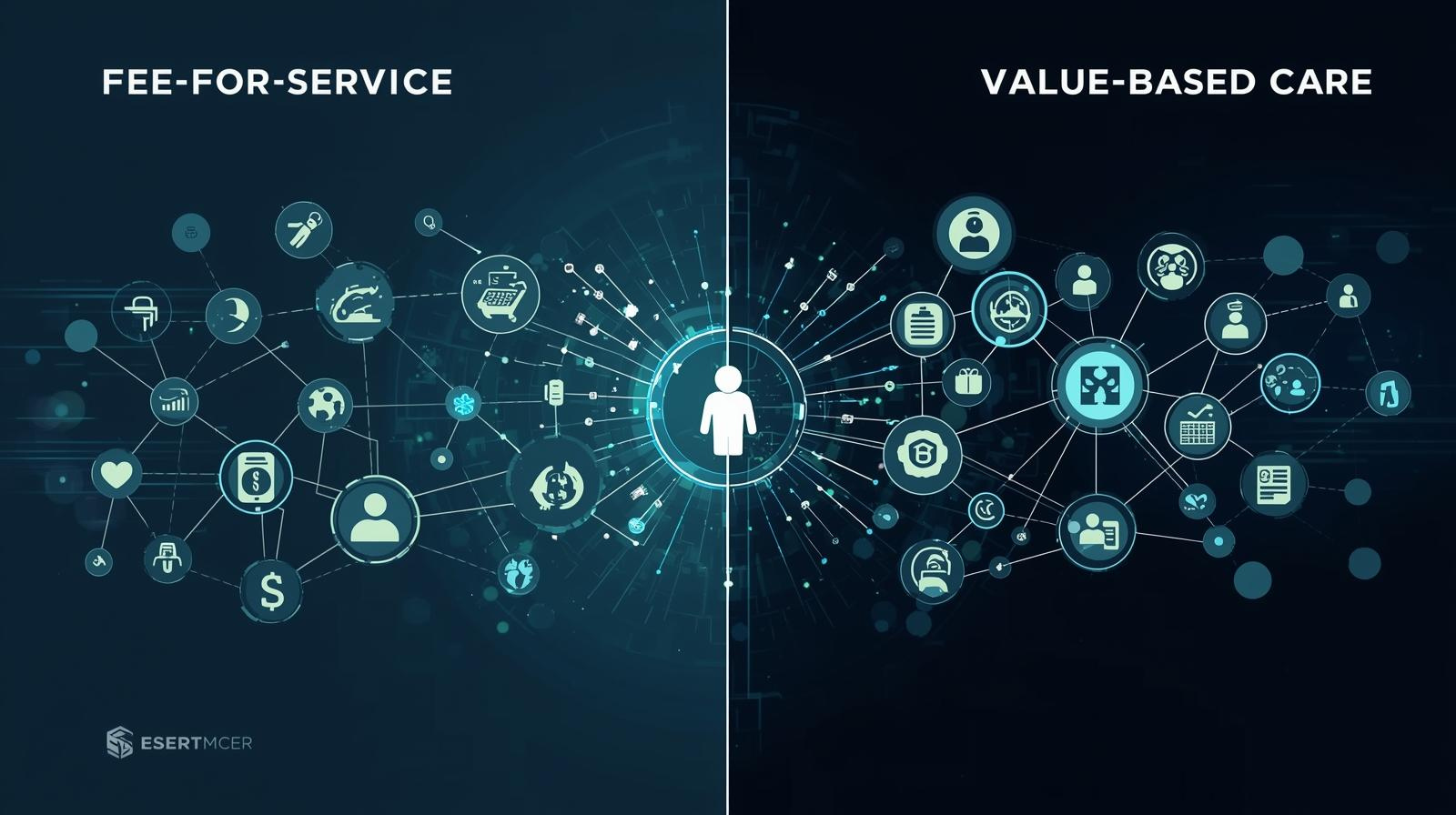
Healthcare payment models define the ways through which providers provide care and the way patients receive treatment. Fee for Service Vs Value-based Care are two prevailing models that embody two totally different philosophies in the medical reimbursement. Fee-for-service is transactional, paying providers for each test, procedure, or visit regardless of the outcome. This model has shaped healthcare for decades, often prioritizing service volume over patient outcomes.
The value-based care changes this equation completely. Providers get rewards for keeping patients healthy, preventing diseases, and attaining positive health outcomes. The shift from counting services to measuring outcomes fundamentally changes how healthcare organizations approach patient care. Knowledge of these differences enables healthcare professionals, administrators, and patients to deal with a changing medical environment in which quality is becoming more important than quantity.
What Makes Fee-for-Service Different from Value-Based Care?
Fee for Service Vs Value-based Care centers on how providers get paid and what behaviors these payment structures encourage. The fundamental distinction affects everything from appointment scheduling to preventive care investment.
In the fee-for-service system, healthcare providers are paid on a per-service basis. These are a blood test, an X-ray, and a consultation that produce different bills and payments. Money is given to the providers according to the amount of services that they provide, and not on how beneficial such services are to the patients.
Value-based care is associated with payment and patient outcomes. Providers get payment as they maintain patient health, effective management of chronic diseases effectively, and reduce hospital readmissions. A provider who helps a diabetic patient avoid an amputation is financially rewarded.
The core differences include:
- Fee-for-service rewards activity while value-based care rewards outcomes
- Fee-for-service measures quantity while value-based care measures quality
- Fee-for-service pays per procedure, while value-based care uses bundled or risk-adjusted payments
- Fee-for-service focuses on treatment, while value-based care emphasizes prevention
This disparity affects every aspect of healthcare service delivery, such as the way doctors schedule their appointments and the amount of money hospitals spend on technology and care coordination initiatives.
1. Payment Structure and Provider Incentives
The provider behavior in healthcare is influenced by payment mechanisms more than any other factor. The manner in which money circulates within the system influences the kind of activities to be given priority, investments that are viable financially, and how providers will spend their time and resources.
How Do Payment Mechanisms Differ?
In the fee-for-service model, providers receive compensation per service. When a physician orders five tests for a patient, he creates five individual payments. The service volume is directly proportional to the revenue, and this forms a tangible monetary impetus to do more billable activities.
Value-based care vs fee-for-service payment structures work oppositely. The bundled payments or risk-sharing systems are given to the providers based on patient outcomes. A healthcare organization may be allocated an amount of money to handle the care of a diabetic patient for a period of a year. They make a profit in case they maintain the lives of that patient and save them from the hospital. In case of complications that are costly to treat, the organization absorbs the cost.
What Behaviors Do These Incentives Create?
Fee-for-service encourages providers to:
- Schedule more frequent follow-up visits
- Order additional diagnostic tests
- Perform procedures with high reimbursement rates
- Focus on treating illness rather than preventing it
Value-based care pushes providers toward:
- Investing in preventive care programs
- Coordinating care across multiple providers
- Using technology to identify high-risk patients early
- Measuring and improving patient satisfaction
The digital health platform is essential in value-based care, enabling providers to track outcomes, organize care teams, and identify patients needing proactive intervention.
2. Quality of Care and Patient Outcomes
The measure of ultimate healthcare effectiveness is patient outcomes. Payment models significantly influence how providers focus on patient health rather than service volume, affecting communication quality and follow-up care consistency.
Does Payment Model Affect Care Quality?
Yes, fee-for-service does not link payment to patient satisfaction. Providers are paid the same regardless of whether patients understand their treatment plans or feel satisfied with care.
Value-based care puts outcomes into the limelight. The providers will be required to show a shift to better health measures of chronic disease cases, lower cases of hospital readmission, better patient satisfaction ratings, and better rates of preventive care follow-ups.
How Do Outcome Measurements Work?
The fee-for-service would monitor the number of patients attended to daily, the number of procedures within the month, and the billing codes that are being filed within the quarter. Value-based care checks the level of HbA1c in diabetic patients, blood pressure management among hypertensive patients, cancer screening baselines, and the quality of life on patient reports.
3. Cost Implications and Financial Sustainability
There is a drastic difference in healthcare spending patterns in payment models. Financial incentives that are inherent in each structure either promote or deter cost-effective care provision, with a direct effect on the sustainability of the system and patient affordability.
How Do Costs Differ Between Models?
Fee-for-service can escalate healthcare spending rapidly. The model creates no financial penalty for unnecessary tests or procedures. A provider ordering ten diagnostic tests when three would suffice receives payment for all ten.
Common cost drivers in the fee-for-service sector comprise duplicate testing where patients meet with several specialists, defensive medicine, costly emergency room care for preventable diseases, and unsuccessful readmission of patients as a result of ineffective discharge planning.
Where Do Cost Savings Come From?
Value-based care vs fee-for-service cost arrangements seek to decrease unwarranted costs. Value-based models develop financial incentives to reduce waste. Those providers who avoid hospital readmissions retain a larger portion of their bundle payment.
Value-based care reduces costs through:
- Preventive care programs that stop diseases before they require expensive treatment
- Care coordination that eliminates duplicate tests and conflicting medications
- Remote monitoring that catches problems before they require hospitalization
- Patient education that helps people manage chronic conditions at home
A healthcare system can invest in preventive measures like foot ultrasounds, nutrition education, and glucose monitoring. While initially costly, these services prevent expensive treatments such as amputations and dialysis, saving money in the long term. Fee-for-service is not conducive to this investment since money used in prevention decreases the procedures that can be billed in the future.
4. Care Coordination and Team Collaboration
The effectiveness of patients requires a smooth interaction between various providers and specialties. This collaboration can be enhanced or slowed by the payment model, which also influences the success of the care teams in working in silo or collaboratively across the board.
Why Does Collaboration Matter More in Value-Based Care?
A patient with diabetes may require the collaboration of a primary care doctor, an endocrinologist, a dietitian, an ophthalmologist, and a podiatrist. These providers, in fee-for-service work, work on their own and attend to their respective services.
Value-based care requires teamwork since collective responsibility is the impetus behind the payment model. When one of the team members does not receive a vital delivery, it affects the entire team by creating poor results and reduced reimbursements.
How Does Care Coordination Work?
Effective coordination requires:
- Shared electronic health records accessible to all team members
- Regular case conferences to discuss complex patients
- Clear protocols for specialist referrals and follow-up
- Patient navigators who help people move through the healthcare system
No reimbursement of coordination activities is made in the context of fee-for-service. Taking time to call other providers, review shared patient records, or even hold a care team meeting does not generate any billable codes. The clinicians in this model tend to operate in isolation, without knowing the activities of the other clinicians on the same patient.
Value-based care makes care coordination financially viable. Bundled and risk-sharing payments cover the time and technology needed to manage care effectively. The healthcare organizations make investments in care management teams, population health tools, and communication systems that make all people aware.
This collaboration extends to partnerships between:
- Hospitals and primary care practices
- Medical providers and social service agencies
- Healthcare systems and community organizations
- Clinical teams and patients themselves as active care partners
5. Prevention Focus and Long-Term Health Management
Preventive measures draw the distinction between reactive care and proactive health care. The payment systems that incentivize staying healthy or pay only when it is time to treat a disease are also at the core of influencing the way that the providers manage the population’s health.
What Role Does Prevention Play in Each Model?
Fee-for-service generates revenue from treating illness rather than preventing it. Prevention reduces billable services, discouraging proactive care. Prevention activities face barriers, including limited reimbursement for counseling time, no payment for population health screening programs, and insufficient compensation for chronic disease management.
Value-based care reverses these incentives entirely. Keeping patients healthy reduces future treatment costs, allowing providers to keep more of their risk-adjusted payments. Prevention becomes a financial strategy rather than a money-losing activity.
How Does Prevention Work in Practice?
Value-based care focuses on screening to diagnose diseases at an early stage before they are harder to cure, chronic disease management initiatives to avoid complications, lifestyle counseling to solve the underlying causes of health issues, and remote monitoring to detect issues before they arise as an emergency.
A value-based primary care practice might implement:
- Annual wellness visits focused on prevention rather than illness
- Care managers who call patients between visits to check on medication adherence
- Group medical appointments where diabetic patients learn from each other
- Home visits for patients with mobility challenges
Fee-for-service practices struggle to justify these investments. The time spent on prevention doesn’t generate sufficient billing codes to cover costs. Value-based payment models render prevention economically viable by linking reimbursement to the long-term health outcomes and not episodic treatment.
Prevention also supports health equity. Value-based care encourages providers to achieve positive outcomes across all patient populations, addressing social determinants such as food insecurity, housing instability, and transportation barriers.
Takeaway
Healthcare organizations need to provide improved performance at reduced costs. The transition of the fee-for-service to the value-based care model necessitates care delivery, technology investment, and performance measurement adjustments. The required success is based on robust data integration, efficient care coordination, and population health instruments that assist in proactive and outcome-based care.
Persivia offers value-based payment technology to organizations migrating towards value-based payment models. The CareSpace® is a platform that consolidates information, reveals the areas of care gaps, and provides actionable insights to enhance quality and financial results. Providers using integrated platforms report better outcomes, lower costs, and more effective care coordination.