Driving Compliance & Speed in Medical Device Teams
Bringing a medical device from concept to clinical use demands coordinated execution across regulatory, clinical, quality, engineering, and commercial functions. The most successful organizations establish cross-functional alignment early especially between R&D, Quality Assurance (QA), and Regulatory Affairs creating a foundation that supports compliance, accelerates development, and reduces costly redesigns. This collaboration is now more critical than ever as the industry prepares for the U.S. FDA’s QMSR harmonization with ISO 13485.
The Unique Complexity of Device Development
Medical-device development is unlike typical software or manufacturing environments because products directly impact patient safety and must satisfy stringent regulatory expectations across the entire product lifecycle. The U.S. FDA’s Quality Management System Regulation (QMSR), which becomes enforceable February 2, 2026, replaces the former Quality System Regulation (QSR) and aligns 21 CFR Part 820 with ISO 13485:2016 principles. This harmonization elevates global consistency while preserving core quality expectations.
For devices subject to design controls most Class II and III devices and a limited subset of Class I 21 CFR 820.30 (and QMSR clause 7.3 after transition) requires structured and documented development processes, all captured in the Design History File (DHF). These artifacts include:
- The Design and Development Plan (DDP)
- Design inputs (user needs, intended use, human-factors considerations)
- Design outputs
- Design reviews
- Verification and validation
- Design transfer to production
- Change control
Given the diversity of disciplines involved regulatory strategists anticipating FDA expectations, engineers executing design solutions, clinicians shaping usability and risk profiles, commercial teams defining positioning cross-functional coordination is essential. Without it, professional “language gaps” (e.g., how statisticians vs. clinicians define “clinical significance”) can lead to misalignment and rework.
Decision Frameworks That Drive Clarity
High-performing teams establish clear decision-making structures from the beginning. While design-control regulations define what must be documented, they do not define how cross-functional teams make decisions. Organizations fill this gap with practical governance tools:
- RACI matricesto define who is responsible, accountable, consulted, and informed.
- Phase-gate or milestone reviewsto ensure cross-functional signoff before advancing.
- Living design plans, updated as the device evolves, maintaining traceability and intent.
- Visible, shared dashboards that give all functions insight into design-history artifacts, risk files, verification progress, and change control.
Clarifying decision authority early prevents cascade bottlenecks for example, uncertainty over who approves trade-offs between performance, safety, and manufacturability.
A primary measure of this governance is maintaining traceability. This is the verifiable link established between Design Inputs (needs, risks) $\rightarrow$ Design Outputs (specifications) $\rightarrow$ Verification/Validation activities (test results) $\rightarrow$ Risk Controls. Maintaining this full traceability matrix is essential for audit readiness.
Collaborative Risk and Usability Management
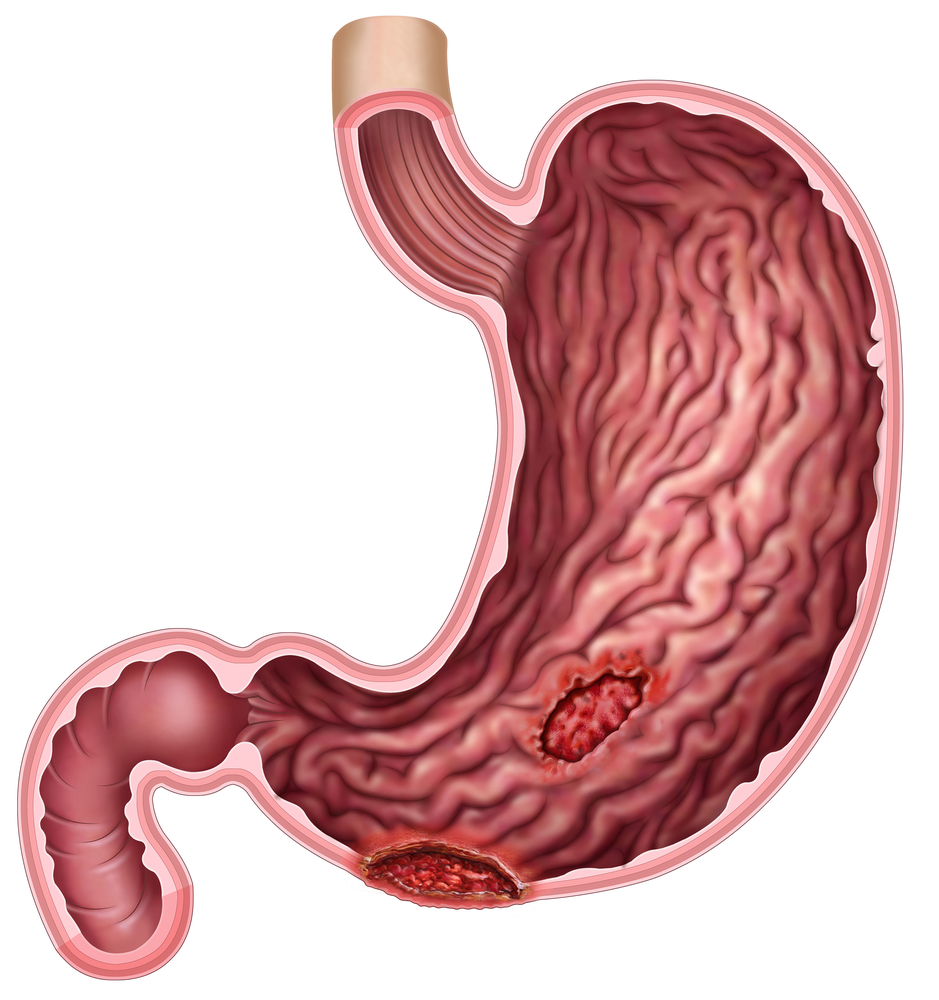
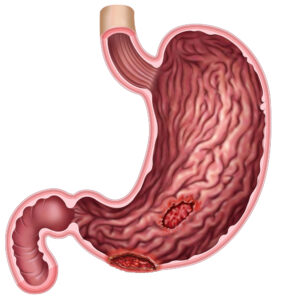
Risk management under ISO 14971 is not a standalone exercise; it is a cross-functional discipline that drives design choices. Furthermore, Human Factors Engineering (HFE) is a critical, distinct function that bridges engineering, clinical, and regulatory needs to mitigate use-related risk (per ISO 62366 and FDA guidance).
Collaborative risk and usability workshops create shared understanding:
- Engineers appreciate regulatory and clinical risk frameworks.
- HFE specialists conduct usability assessments and highlight potential use errors.
- Clinical leaders highlight patient, workflow, and usability risks grounded in real-world scenarios.
- Quality and Regulatory teams ensure alignment with hazard-analysis, traceability, and verification evidence.
Design-control gaps and poor risk integration are frequently cited in FDA findings and contribute to many late-stage redesigns. Early alignment reduces redesign cycles and strengthens regulatory submissions. Modern cloud-enabled Quality Management System (QMS) tools, though not required, help organizations maintain single-source-of-truth documentation, structured workflows, and audit-ready records significantly reducing the compliance burden.
The Bridge Role of Clinical Leadership
Clinical leadership plays a unique integrative role at the intersection of engineering, regulatory strategy, human factors, and commercial relevance. Clinicians help translate device capabilities into:
- Patient-centered requirements and realistic workflow needs.
- Benefit-risk reasoning in line with FDA expectations.
- Clear clinical evidence strategies, including planning for Post-Market Clinical Follow-up (PMCF).
- Messaging aligned with provider value and market differentiation.
Because design inputs must reflect intended use, user needs, and human-factors considerations, clinical leadership ensures these are grounded in real-world patient care and provider behavior. This perspective is vital for ensuring the device is designed not just to be functional, but to be safe and effective in its intended environment.
Lifecycle Alignment: From Concept to Post-Market
Medical-device development progresses through concept, feasibility, verification/validation, clinical evaluation, regulatory submission, and commercialization. While formal design controls generally begin once a firm commits to development, early rapid prototyping provides invaluable insight.
Using real hardware, edge-case scenarios, and preliminary usability testing, teams can uncover issues early before formal requirements harden. Once design controls are active, disciplined phase-gate transitions maintain alignment.
Crucially, modern global regulations, particularly the EU MDR, demand that clinical, regulatory, and quality teams establish robust Post-Market Surveillance (PMS) plans during early development. This ensures that the mechanisms for collecting safety, performance, and PMCF data are built into the device design and the organization’s QMS processes from the start. Design transfer (21 CFR 820.30(h)) then ensures that validated design outputs are translated into production specifications without disconnects between engineering intent and manufacturing reality.
Psychological Safety as a Quality Enabler
In regulated environments, psychological safety is not a cultural luxury it is a compliance advantage. Teams that feel safe escalating uncertainties, raising safety signals, or admitting knowledge gaps surface defects earlier and produce stronger design-history evidence. Leaders reinforce this by:
- Explaining rationales behind decisions.
- Recognizing early issue-spotters.
- Encouraging constructive dissent.
- Structuring meetings to give equal voice across disciplines.
This environment reduces late-stage changes, which often trigger verification rework or delay regulatory submissions.
The Evolving Collaboration Landscape
Regulatory expectations are expanding as technology advances and harmonization accelerates.
- QMSRharmonizes U.S. quality expectations with global norms.
- AI/ML-enabled devices and SaMD introduce continuous-learning, human-factors, and cybersecurity considerations.
- EU MDR and upcoming AI Act requirements push teams toward more integrated post-market surveillance, data governance, and lifecycle-risk documentation.
Cross-functional governance is becoming a competitive differentiator, not just a compliance necessity. Strong coordination ensures strong evidence planning, accelerating access to breakthrough programs and managing the evolving complexity of digital health.
Conclusion
In an era where regulatory expectations, technological complexity, and global harmonization are accelerating, cross-functional excellence determines whether a device reaches patients on time and with the safety and performance they deserve. Organizations that treat plans as living documents, invest early in collaborative risk management, and unify engineering, clinical, regulatory, and quality perspectives transform development complexity into meaningful patient impact.